Uterine Conditions & Treatment
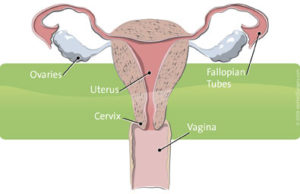
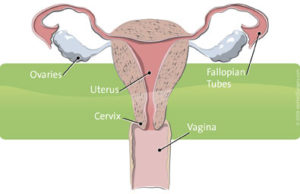
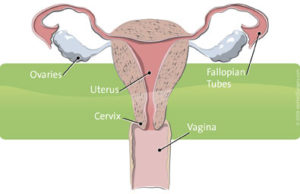
When a woman faces a medical condition that affects her uterus, the hollow, muscular organ that holds and feeds a fertilized egg, the emotional impact can often be as challenging as the physical. These conditions include, but are not limited to, cervical and uterine cancers such as endometrial cancer, uterine fibroids, uterine prolapse, excessive bleeding and endometriosis.
Treatment options are as varied as the conditions themselves, depending on individual circumstances. A woman’s age, health history, surgical history and diagnosis (benign or cancerous), all factor into the recommended course of action.
Endometriosis, also known as endometrial hyperplasia, is a condition in which the endometrial tissue grows outside the uterus, causing scarring, pain, and heavy bleeding. It can often damaging the fallopian tubes and ovaries in the process. A common organic cause of infertility, endometriosis can be treated with medications such as lupron for endometriosis that lowers hormone levels and decreases endometrial growths. While such medications often relieve associated symptoms, a patient should understand the potential side effects before pursuing this treatment regimen.
For endometrial cancer, also known as uterine cancer and more common among women after menopause, standard treatment options include hormone therapy, radiation therapy, chemotherapy and hysterectomy (surgical removal of the uterus). Three of these — radiation therapy, chemotherapy and hysterectomy — are also used to treat cervical cancer.
For benign (non-cancerous) conditions like menorrhagia (heavy menstrual bleeding), non-surgical treatments like hormone therapy or minimally invasive ablative therapies may offer relief. For fibroids, uterine-preserving myomectomy – a surgical alternative to hysterectomy — may be an option.
Hysterectomy
For most uterine conditions, if available non-surgical treatments fail to relieve symptoms, many women choose a more certain result with elective hysterectomy. Each year in the U.S. alone, doctors perform about 600,000 hysterectomies, making it the second most common surgical procedure.1
While symptoms such as chronic pain and bleeding often point a woman and her doctor toward hysterectomy as the preferred treatment choice, life-threatening conditions such as cancer or uncontrollable bleeding in the uterus often necessitate a hysterectomy and follow-up treatment.
While hysterectomy is relatively safe, always ask your doctor about all treatment options, as well as their risks and benefits, to determine which approach is right for you. And if hysterectomy is recommended or required, you owe it to yourself to learn about da Vinci Hysterectomy, a robot-assisted, minimally invasive surgery that for many women has potential as the safest and most effective treatment available.
1.Center for Disease Control. Keshavarz H, Hillis S, Kieke B, Marchbanks P. Hysterectomy Surveillance — United States, 1994–1999. Morbidity and Mortality Weekly Report. Surveillance Summaries. July 12, 2002. Vol. 51 / SS-5. Page 1. www.cdc.gov/mmwr/PDF/ss/ss5105.pdf
While clinical studies support the effectiveness of the da Vinci® System when used in minimally invasive surgery, individual results may vary. Surgery with the da Vinci Surgical System may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits.
For additional information on minimally invasive surgery with the da Vinci® Surgical System visit www.davincisurgery.com
Fibroids & Treatment Options
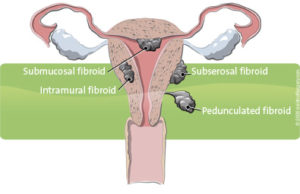
Uterine fibroids* are benign (non-cancerous) tumors occurring in at least one quarter of all women.1 They can grow underneath the uterine lining, inside the uterine wall, or outside the uterus.
Many women don’t feel any symptoms with uterine tumors or fibroids. But for others, these fibroids can cause excessive menstrual bleeding (also called menorrhagia), abnormal periods, uterine bleeding, pain, discomfort, frequent urination and infertility.2
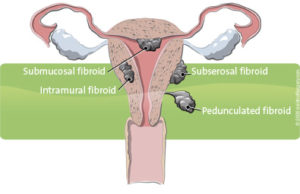
Treatments include uterine fibroid embolization – which shrinks the tumor – and surgery. Surgical treatment for uterine tumors most often involves the surgeon removing the entire uterus, via hysterectomy.3
While hysterectomy is a proven way to resolve fibroids, it may not be the best surgical treatment for every woman. If, for example, you hope to later become pregnant, you may want to consider alternatives to hysterectomy like myomectomy. Myomectomy is a uterine-preserving procedure performed to remove uterine fibroids.
Types of Myomectomy
Each year, roughly 65,000 myomectomies are performed in the U.S.4 The conventional approach to myomectomy is open surgery, through a large abdominal incision.5 After cutting around and removing each uterine fibroid, the surgeon must carefully repair the uterine wall to minimize potential uterine bleeding, infection and scarring. Proper repair is also critical to reducing the risk of uterine rupture during future pregnancies. Menorrhagia is extensive menstrual bleeding.
While myomectomy is also performed laparoscopically, this approach can be challenging for the surgeon, and may compromise results compared to open surgery.6 Laparoscopic myomectomies often take longer than open abdominal myomectomies, and up to 28% are converted during surgery to an open abdominal incision.7
A new category of minimally invasive myomectomy, da Vinci®Myomectomy, combines the best of open and laparoscopic surgery. With the assistance of the da Vinci Surgical System – the latest evolution in robotics technology – surgeons may remove uterine fibroids through small incisions with unmatched precision and control.
* Uterine fibroids are also called fibroids, uterine tumors, leiomyomata (singular – leiomyoma) and myomas or myomata (singular – myoma)
1.Newbold RR, DiAugustine RP, Risinger JI, Everitt JI, Walmer DK, Parrott EC, Dixon D. Advances in uterine leiomyoma research: conference overview, summary, and future research recommendations. Environ Health Perspect. 2000 Oct;108 Suppl 5:769-73. Review.
2.National Institutes of Health: Fast Facts about Uterine Fibroids. www.nichd.nih.gov/publications/pubs/fibroids/sub1.htm#where
3.Becker ER, Spalding J, DuChane J, Horowitz IR. Inpatient surgical treatment patterns for patients with uterine fibroids in the United States, 1998-2002. J Natl Med Assoc. 2005 Oct;97(10):1336-42.
4.Lumsden MA.Embolization versus myomectomy versus hysterectomy: Which is best, when? Hum Reprod. 2002; 17:253-259. Review.
5.Becker ER, Spalding J, DuChane J, Horowitz IR. Inpatient surgical treatment patterns for patients with uterine fibroids in the United States, 1998-2002. J Natl Med Assoc. 2005 Oct;97(10):1336-42.
6.Kristen A. Wolanske, MD; Roy L. Gordon, MD. Uterine Artery Embolization: Where Does it Stand in the Management of Uterine Leiomyomas? Part 2. Appl Radiol33(10):18-25, 2004. Medscape.10/27/2004.
7.Advincula AP, Song A, Burke W, Reynolds RK. Preliminary experience with robot-assisted laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004 Nov;11(4):511-8.
While clinical studies support the effectiveness of the da Vinci® System when used in minimally invasive surgery, individual results may vary. Surgery with the da Vinci Surgical System may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits.
For additional information on minimally invasive surgery with the da Vinci® Surgical System visit www.davincisurgery.com
Hysterectomy
Physicians perform hysterectomy – the surgical removal of the uterus – to treat a wide variety of uterine conditions. Each year in the U.S. alone, doctors perform approximately 600,000 hysterectomies, making it the second most common surgical procedure.1
Types of Hysterectomy
There are various types of hysterectomy that are performed depending on the patient’s diagnosis:
- Supracervical hysterectomy – removes the uterus, leaves cervix intact
- Total hysterectomy – removes the uterus and cervix
- Radical hysterectomy or modified radical hysterectomy – a more extensive surgery for gynecologic cancer that includes removing the uterus and cervix and may also remove part of the vagina, fallopian tubes, ovaries and lymph nodes in order to stage the cancer (determine how far it has spread).
Approaches to Hysterectomy
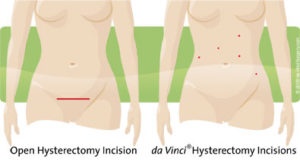
Surgeons perform the majority of hysterectomies using an “open” approach, which is through a large abdominal incision. An open approach to the hysterectomy procedure requires a 6-12 inch incision. When cancer is involved, the conventional treatment has always been open surgery using a large abdominal incision, in order to see and, if necessary, remove related structures like the cervix or the ovaries.
A second approach to hysterectomy, vaginal hysterectomy, involves removal of the uterus through the vagina, without any external incision or subsequent scarring. Surgeons most often use this minimally invasive approach if the patient’s condition is benign (non-cancerous), when the uterus is normal size and the condition is limited to the uterus.
In laparoscopic hysterectomy, the uterus is removed either vaginally or through small incisions made in the abdomen. The surgeon can see the target anatomy on a standard 2D video monitor thanks to a miniaturized camera, inserted into the abdomen through the small incisions. A laparoscopic approach offers surgeons better visualization of affected structures than either vaginal or abdominal hysterectomy alone.
While minimally invasive vaginal and laparoscopic hysterectomies offer obvious potential advantages to patients over open abdominal hysterectomy – including reduced risk for complications, a shorter hospitalization and faster recovery – there are inherent drawbacks. With vaginal hysterectomy, surgeons are challenged by a small working space and lack of view to the pelvic organs. Additional conditions can make the vaginal approach difficult, including when the patient has:
- A narrow pubic arch (an area between the hip bones where they come together)2
- Thick adhesions due to prior pelvic surgery, such as C-section3
- Severe endometriosis 4
- Non-localized cancer (cancer outside the uterus) requiring more extensive tissue removal, including lymph nodes
With laparoscopic hysterectomy, surgeons may be limited in their dexterity and by 2D visualization, potentially reducing the surgeon’s precision and control when compared with traditional abdominal surgery.
da Vinci Hysterectomy
A new, minimally invasive approach to hysterectomy, da VinciHysterectomy, combines the advantages of conventional open and minimally invasive hysterectomies – but with far fewer drawbacks. da VinciHysterectomy is becoming the treatment of choice for many surgeons worldwide. It is performed using the da Vinci System, which enables surgeons to perform surgicall procedures with unmatched precision, dexterity and control. Read about what may be the most effective, least invasive approach to hysterectomy .
1.Center for Disease Control. Keshavarz H, Hillis S, Kieke B, Marchbanks P. Hysterectomy Surveillance — United States, 1994–1999. Morbidity and Mortality Weekly Report. Surveillance Summaries. July 12, 2002. Vol. 51 / SS-5. Page 1. www.cdc.gov/mmwr/PDF/ss/ss5105.pdf
2.Harmanli OH, Khilnani R, Dandolu V, Chatwani AJ. Narrow pubic arch and increased risk of failure for vaginal hysterectomy. Obstet Gynecol. 2004 Oct;104(4):697-700.
3.Paparella P, Sizzi O, Rossetti A, De Benedittis F, Paparella R. Vaginal hysterectomy in generally considered contraindications to vaginal surgery. Arch Gynecol Obstet. 2004 Sep;270(2):104-9. Epub 2003 Jul 10.
4.Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials.BMJ. 2005 Jun 25;330(7506):1478. Review.
While clinical studies support the effectiveness of the da Vinci® System when used in minimally invasive surgery, individual results may vary. Surgery with the da Vinci Surgical System may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits.
For additional information on minimally invasive surgery with the da Vinci® Surgical System visit www.davincisurgery.com
da Vinci Hysterectomy
If your doctor recommends hysterectomy, you may be a candidate for da Vinci Hysterectomy, one of the most effective, least invasive treatment options for a range of uterine conditions. da Vinci Hysterectomy is performed using the da Vinci™ Surgical System, which enables surgeons to perform with unmatched precision and control – using only a few small incisions.
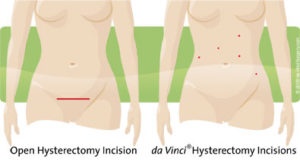
For most patients, da Vinci Hysterectomy can offer numerous potential benefits over traditional approaches to vaginal, laparoscopic or open abdominal hysterectomy, particularly when performing more challenging procedures like radical hysterectomy for gynecologic cancer. Potential benefits include:
- Significantly less pain
- Less blood loss
- Fewer complications
- Less scarring
- A shorter hospital stay
- A faster return to normal daily activities
Moreover, da Vinci provides the surgeon with a superior surgical tool for dissection and removal of lymph nodes during cancer operations, as compared to traditional open or minimally invasive approaches.1 da VinciHysterectomy also allows your surgeon better visualization of anatomy, which is especially critical when working around delicate and confined structures like the bladder. This means that surgeons have a distinct advantage when performing a complex, radical hysterectomy involving adhesions from prior pelvic surgery or non-localized cancer, or an abdominal hysterectomy. 2
As with any surgery, these benefits cannot be guaranteed, as surgery is both patient- and procedure-specific. While radical hysterectomy or abdominal hysterectomy performed using the da Vinci Surgical System are considered safe and effective, these procedures may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits.
1.Boggess JF. da Vinci® Hysterectomy for Endometrial Cancer with Staging. Presented at ISI WWSSM 1/06. 871391_rev B_dVH Endometrial Cancer Presentation
2. UNC Department of Obstetric & Gynecology Health & Healing in the Triangle Vol 8 No 3 pp 22-23.
Clinical References
The following selected publications support the clinical efficacy of da Vinci®Gynecologic Surgery. For additional citations on robotic surgery, please visit PubMed (Medline).
Please note: PubMed provides links to downloadable PDFs, which are usually available from the journal publisher for a fee. You may also contact academic libraries (for example, University of California) and inquire about their document delivery services.
da Vinci Hysterectomy for Benign Conditions
2007
John F. Boggess, Paola A. Gehrig, Victoria Bae-Jump, Lisa Abaid, Aaron Shafer, Daniel Clarke-Pearson, Teresa L. Rutledge, John T. Soper, Linda Van Le, Wesley C. Fowler, Jr. Robotic Assistance Improves Minimally Invasive Surgery For Endometrial Cancer. Poster presented at SGO 2007. Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill.
Senapati S, Advincula A. Surgical techniques: robot-assisted laparoscopic Myomectomy with the da Vinci® surgical system. J Robotic Surg. 2007 March; 1(1): 69-74. Abstract. Full text.
2006
Advincula AP. Surgical techniques: robot-assisted laparoscopic hysterectomy with the da Vinci surgical system. Int J Med Robot. 2006 Dec;2(4):305-11. Abstract.
2005
Advincula AP, Reynolds RK. The use of robot-assisted laparoscopic hysterectomy in the patient with a scarred or obliterated anterior cul-de-sac. JSLS. 2005 Jul-Sep;9(3):287-91. Abstract.
Beste TM, Nelson KH, Daucher JA. Total laparoscopic hysterectomy utilizing a robotic surgical system. JSLS. 2005 Jan-Mar; 9(1): 13-15.Abstract.
Marchal F, Rauch P, Vandromme J, Laurent I, Lobontiu A, Ahcel B, Verhaeghe JL, Meistelman C, Degueldre M, Villemot JP, Guillemin F. Telerobotic-assisted laparoscopic hysterectomy for benign and oncologic pathologies: initial clinical experience with 30 patients. Telerobotic-assisted laparoscopic hysterectomy for benign and oncologic pathologies: initial clinical experience with 30 patients. Surg Endosc. 2005 May 3 [Epub ahead of print] Abstract.
2004
Advincula AP, Falcone T. Laparoscopic robotic gynecologic surgery. Obstet Gynecol Clin North Am. 2004 Sep; 31(3): 599-609. Abstract.
Ferguson JL, Beste TM, Nelson KH, Daucher JA. Making the transition from standard gynecologic laparoscopy to robotic laparoscopy. JSLS. 2004 Oct-Dec; 8(4): 326-328. Abstract.
2002
Diaz-Arrastia C, Jurnalov C, Gomez G, Townsend C Jr. Laparoscopic hysterectomy using a computer-enhanced surgical robot. Surg Endosc.2002 Sep; 16(9): 1271-1273. Abstract.
Falcone T, Steiner CP. Robotically assisted gynaecological surgery. Hum Fertil (Camb). 2002 May; 5(2): 72-74. Abstract.
da Vinci Hysterectomy for Early Stage Gynecological Cancer
Boggess JF. Robotic surgery in gynecologic oncology: evolution of a new surgical paradigm J Robotic Surg. 2007 March; 1(1): 69-74. Abstract. Full text.
Aaron Shafer, John F. Boggess, Paola Gehrig, Victoria Bae-Jump, Lisa Abaid, Daniel Clarke-Pearson, Wesley C. Fowler Jr., Teresa L. Rutledge, John Soper, Linda Van Le. Type III radical hysterectomy for obese women with cervical carcinoma: Robotic versus open. Abstract presented at SGO 2007. University of North Carolina, Chapel Hill, NC.
Lynn D. Kowalski, MD, Camille A. Falkner, MD, Stephanie A. Wishnev, MD Nevada Surgery and Cancer Care 1 Sunrise Hospital and Medical Center, Las Vegas, NV. Incorporation of Robotics into a Gynecologic Oncology Practice: The First 100 Cases. Poster presented at SGO 2007.
da Vinci Myomectomy
Advincula AP, Song A, Burke W, Reynolds RK. Preliminary experience with robot-assisted laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004 Nov;11(4):511-8. Abstract.
Bocca S, Stadtmauer L, Oehninger S. Uncomplicated full term pregnancy after da Vinci-assisted laparoscopic myomectomy. Reprod Biomed Online. 2007 Feb;14(2):246-9. Abstract.
Dharia SP, Falcone T. Robotics in reproductive medicine. Fertil Steril. 2005 Jul;84(1):1-11. Review. Abstract.
da Vinci Sacrocolpopexy
Di Marco DS, Chow GK, Gettman MT, Elliott DS. Robotic-assisted laparoscopic sacrocolpopexy for treatment of vaginal vault prolapse.Urology. 2004 Feb; 63(2): 373-376. Abstract.
Elliott DS, Chow GK, Gettman M. Current status of robotics in female urology and gynecology. World J Urol. 2006 Jun;24(2):188-92. Epub 2006 Mar 24. Abstract.
Elliott DS, Krambeck AE, Chow GK. Long-term results of robotic assisted laparoscopic sacrocolpopexy for the treatment of high grade vaginal vault prolapse. J Urol. 2006 Aug;176(2):655-9. Abstract.